|
Show all abstracts
??Show selected abstracts??
??Add to my list
|
|
| EDITORIALS |
? |
|
|
Odontogenic cysts |
p. 101 |
Rafaela Scariot de Moraes, Bruno Tochetto Primo
DOI:10.4103/2278-9588.121837?? |
| [HTML Full text]??[PDF]??[Mobile Full text]??[EPub]??[Sword Plugin for Repository]Beta
|
|
|
|
|
|
|
Standards of care for patients with orofacial clefts in Brazil |
p. 103 |
Sivakumar Nuvvula
DOI:10.4103/2278-9588.121838?? |
| [HTML Full text]??[PDF]??[Mobile Full text]??[EPub]??[Sword Plugin for Repository]Beta
|
|
|
|
|
|
|
| ORIGINAL ARTICLES |
 |
|
|
|
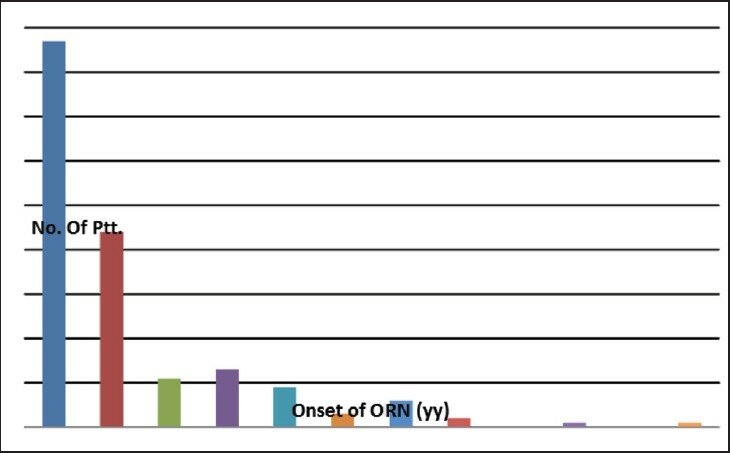
Osteoradionecrosis: Patient characteristics and treatment outcome in a cohort from Copenhagen University Hospital 1995-2005 |
p. 105 |
Rannvá Matras, Lone Forner, Elo Andersen, Lena Specht, Søren Hillerup
DOI:10.4103/2278-9588.121840??
Purpose: The present retrospective observational study was undertaken to evaluate disease characteristics, treatment strategy and treatment results of a large unselected cohort of patients with osteoradionecrosis (ORN) after radiation therapy (RT) for head and neck cancer at the Copenhagen University Hospital 1995-2005. Patients and Methods: Medical records of 180 consecutive patients diagnosed with ORN were reviewed. Patients had all received treatment for ORN at the Department of Oral Maxillofacial Surgery, Copenhagen University Hospital from 1 January 1995 to 31 December 2005. Only patients who had received their primary treatment for head and neck cancer in the eastern part of Denmark were included. Results: The cohort consisted predominantly of men (78%) of whom a clear majority were smokers (60.6%). The median age was 57. The median time until the onset of post-RT ORN was 1.9 years. ORN lesions were mostly located in the mandibular symphysis, body and angle regions. Hyperbaric oxygen treatment was given to 93% of the patients; and 25% of the patients completed disease-free follow-up after a median of 1.2 years. At the time of study termination, 17% were still undergoing active treatment. Social class distribution showed a clear predominance of the lower social classes. Conclusion: The present study demonstrates the variability of mandibular ORN. Onset varies greatly, which demonstrates the lifelong nature of the risk of ORN. In the majority of patients, the primary tumor was located in the oral cavity or the oropharynx. ORN does not appear to imply social inequality.
|
| [ABSTRACT]??[HTML Full text]??[PDF]??[Mobile Full text]??[EPub]??[Sword Plugin for Repository]Beta
|
|
|
|
|
|
|
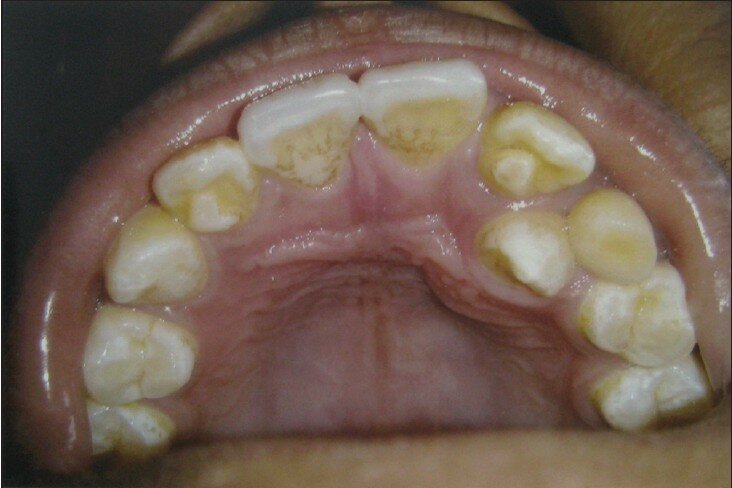
Prevalence of talon cusp in the North Indian population |
p. 114 |
Santosh R Patil, Sneha Maheshwari, Suneet Khandelwal
DOI:10.4103/2278-9588.121841??
Aim: Talon cusp is an uncommon dental anomaly seen commonly in the maxillary anterior. Mostly asymptomatic, it can result in functional and esthetic problems. The aim of the present study was to determine the prevalence of talon cusp in the North Indian population. Materials and Methods: The data was collected from the radiographic examination of 6048 periapical films showing 18,754 teeth from a random sample of 3320 patients attending the Department of Oral Medicine and Radiology. A tooth with a superimposed V-shape radiopaque structure was considered having a talon cusp. Results: Talon cusp was detected in 122 teeth with a tooth prevalence of 0.65. Maxillary lateral incisors were the most commonly affected teeth (86 teeth, 70.5%), followed by maxillary canines (24 teeth, 19.7%) and maxillary central incisors (12 teeth, 9.8%). None of the patients had talon cusp in the mandibular teeth. The person prevalence was estimated at 2.95. Bilateral talon cusp was found in 24 patients. Conclusion: Talon's cusp is a rare clinically evident dental anomaly. Careful observation during the routine dental examination can help in the early diagnosis of talon cusp and associated anomalies. This can help prevent the associated treatment problems and further complications.
|
| [ABSTRACT]??[HTML Full text]??[PDF]??[Mobile Full text]??[EPub]??[Sword Plugin for Repository]Beta
|
|
|
|
|
|
|
| COMMENTARY |
 |
|
|
|
Commentary |
p. 119 |
| Prasanna Kumar Rao |
| [HTML Full text]??[PDF]??[Mobile Full text]??[EPub]??[Sword Plugin for Repository]Beta
|
|
|
|
|
|
|
Commentary |
p. 120 |
| Thirumalaisamy Elangovan |
| [HTML Full text]??[PDF]??[Mobile Full text]??[EPub]??[Sword Plugin for Repository]Beta
|
|
|
|
|
|
|
| ORIGINAL ARTICLES |
 |
|
|
|
Standards of care for patients with orofacial clefts in Brazil: Starting a necessary debate |
p. 122 |
Fernanda C Queirós, George L Wehby, Camila Vila-Nova, Luzia Poliana A Silva
DOI:10.4103/2278-9588.121844??
Background: Unwarranted variation in the provision of health-care services for patients with orofacial clefts (OFC) may exist both within and between countries. Establishing standards of care (SOC) can reduce this variation and improve patient outcomes. Aim: The aim of this study is to describe SOC for treatment and longitudinal evaluation of individuals with OFC in selected craniofacial centers in Brazil compared with standards established by the American Cleft Palate-Craniofacial Association (ACPA). Materials and Methods: This was a descriptive pilot study. A professional from the participating craniofacial centers, who had adequate knowledge about SOC at their institutions, completed a web survey. Results: Eight craniofacial centers, including the five largest centers for cleft care in Brazil, answered the web-survey. All centers follow the ACPA minimum parameters for team composition. However, only one center follows all recommendations for longitudinal evaluation and treatment of patients. Four centers meet all but one recommendation. Age at bone grafting of the alveolar cleft and instrumental assessment of velopharyngeal function were the two most varying parameters from ACPA standards, with only about half of studied centers adhering to them. There were no clear patterns of variation in adherence by facility location, size and years since the establishment. Conclusion: The large variation between centers in treatment and longitudinal evaluation protocols highlights the need to adopt similar SOC for individuals with orofacial clefts in Brazil and to identify barriers for adopting these standards.
|
| [ABSTRACT]??[HTML Full text]??[PDF]??[Mobile Full text]??[EPub]??[Sword Plugin for Repository]Beta
|
|
|
|
|
|
|
Malignant otitis externa: Cranial nerve palsies, skull-base erosions and prognosis |
p. 130 |
Mohammad Shaheryar Ahmed Rajput, Asif Ali Arain, M Sohail Awan, Shabbir Akhter, Mohammad Adeel
DOI:10.4103/2278-9588.121845??
Introduction: Malignant otitis externa (MOE) is an infection of the temporal bone usually affecting elderly diabetic patients, which can potentially be life threatening. The causative organism is most commonly Pseudomonas aeruginosa. Objective: Objective of the study was to review our experience of managing patients with MOE. The second objective was to compare the outcome of patients with and without cranial nerve paralysis and bony erosions evident on computed tomography (CT?) scan. Materials and Methods: Our departmental database was searched for all patients hospitalized with the diagnosis of MOE between January 2000 and December 2009. A total of 21 patients were included in the study based on our inclusion criteria. Variables studied were: Clinical features including edema and granulations in external auditory canal (EAC), presence of otalgia, exudate, bony erosions of EAC, mastoid or petrous apex on CT scan and diabetes mellitus or other immunocompromised state. Outcome was assessed in terms of mortality and cure. Fisher's exact test was applied to find out effect of nerve palsies and bony erosions on outcome. Result and Conclusion: MOE is an aggressive and life-threatening infection. The mortality rate was found to be 14.3%. Analysis of findings revealed no statistically significant effect of temporal bone erosions and neuropathies on outcome.
|
| [ABSTRACT]??[HTML Full text]??[PDF]??[Mobile Full text]??[EPub]??[Sword Plugin for Repository]Beta
|
|
|
|
|
|
|
Cytomorphometric analysis of the keratinocytes obtained from clinically normal buccal mucosa in chronic gutkha chewers |
p. 134 |
Swetha Acharya, S Amsavardani Tayaar, Tahura Khwaja
DOI:10.4103/2278-9588.121846??
Objective: The objective of this study was to examine the cellular changes induced by chronic gutkha chewing in buccal mucosa as revealed by cytomorphometry. Study design: Nuclear area (NA), cellular area (CA), nuclear diameter (ND), cellular diameter (CD), ratio of NA to CA (NA:CA), ratio of ND to CD (ND:CD) of exfoliated buccal squames obtained from clinically normal appearing buccal mucosa of chronic gutkha chewers (n = 30), were stained by Papanicolou method and observed under light microscope. 100 cells in each case were measured using image analyser. Non-gutkha users (healthy) served as negative controls (n = 20) and oral squamous cell carcinomas (OSCCs) in gutkha users served as positive controls (n = 20). All the variables except for ND:CD (using Shapero-Wilk test) were normally distributed and hence their mean difference was tested using ANOVA followed by Tukey test. In case of ND:CD non-parametric Kruskal-Wallis test followed by Mann-Whitney test was applied. Results: A highly significant decrease in CD, CA, increase in ND, NA, ND:CD and NA:CA were observed in smears obtained from chronic gutkha chewers when compared with the healthy controls (P < 0.05). The mean value of ND and NA in gutkha chewers was greater than those of healthy controls, but lesser than that of OSCC cases. Conversely, the CD and CA gradually decreased from healthy controls to gutkha chewers to OSCC cases. Conclusions: The findings indicate that gutkha chewing influences the cellular alterations. The study confirms cytomorphometric changes in the buccal keratinocytes of chronic gutkha chewers.
|
| [ABSTRACT]??[HTML Full text]??[PDF]??[Mobile Full text]??[EPub]??[Sword Plugin for Repository]Beta
|
|
|
|
|
|
|
| REVIEW ARTICLE |
 |
|
|
|
Update on Langerhans cells |
p. 142 |
Robin Sabharwal, Shamindra Sengupta, Bhudev Sharma, Vineet Gupta
DOI:10.4103/2278-9588.121847??
The Langerhans cells (LC) are the bone marrow-derived dendritic, antigen-presenting cells of the skin and oral mucosa. These are characterized by a unique intra cytoplasmic organelle - the Birbeck granule and constitutively expresses class II major histocompatibility complex (MHC) molecules and the Cluster differentiation Ia (CD1a) glycoprotein. The LC represents one of the most potent APC of the body and fulfills an important role in detecting foreign antigen entering the body through the skin and in immune surveillance. The distribution of LC is restricted to the skin, lymph nodes, bronchial mucosa, and thymus. This paper reviews the classification, origin, and the role of the LC in various pathological conditions.
|
| [ABSTRACT]??[HTML Full text]??[PDF]??[Mobile Full text]??[EPub]??[Sword Plugin for Repository]Beta
|
|
|
|
|
|
|
| COMMENTARY |
 |
|
|
|
Commentary |
p. 149 |
| Ichiro Murakami |
| [HTML Full text]??[PDF]??[Mobile Full text]??[EPub]??[Sword Plugin for Repository]Beta
|
|
|
|
|
|
|
| CASE REPORTS |
 |
|
|
|
Bilateral conductive hearing loss due to facial canal overlying on the oval window |
p. 151 |
Rifat Karli
DOI:10.4103/2278-9588.121849??
The facial canal (FC) may display congenital bony dehiscences, and the facial nerve may show variations and anomalies of its usual course. These features have clinical and surgical significance. The aim of this study is to report FC course anomalies overlying the oval window in a patient presenting with conductive hearing loss and FC dehiscence.
|
| [ABSTRACT]??[HTML Full text]??[PDF]??[Mobile Full text]??[EPub]??[Sword Plugin for Repository]Beta
|
|
|
|
|
|
|
Ramsay Hunt syndrome with cranial polyneuropathy |
p. 154 |
Rachana V Prabhu, Preeti Volvoikar, Ajit Dinkar, Vishnudas D Prabhu
DOI:10.4103/2278-9588.121850??
Ramsay Hunt syndrome (RHS), also known as Zoster Oticus, is a rare complication of Herpes Zoster, in which there is reactivation of latent varicella zoster virus infection in the geniculate ganglion. RHS with involvement of other cranial nerves is a rare finding. Very few cases of RHS with cranial polyneuropathy have been reported in the literature. A successfully treated case of RHS with cranial polyneuropathy of V, VII, VIII, and IX cranial nerves has been reported.
|
| [ABSTRACT]??[HTML Full text]??[PDF]??[Mobile Full text]??[EPub]??[Sword Plugin for Repository]Beta
|
|
|
|
|
|
|
Primary intraosseous squamous cell carcinoma of mandible ex-odontogenic cyst in a young patient |
p. 158 |
Shraddha Jain, Ansu Sam, Dennis I Yohannan, Sunil Kumar, Deepti Joshi, Madhu Priya
DOI:10.4103/2278-9588.121851??
We report a case of primary intraosseous carcinoma (PIOC) of the mandible arising from the epithelial lining of pre-existing odontogenic cyst in a 21-year-old male who presented with external swelling in the region of body and ramus of right mandible, pain, spontaneous shedding of right third molar tooth, and difficulty in opening the jaw. Contrast-enhanced computed tomography of head and neck region showed an expansile unilocular lesion with mixed solid and cystic components involving the right hemimandible in both its ramus and body with widening of the mental foramen and soft-tissue extension anteriorly suggestive of perineural invasion. The patient underwent right hemimandibulectomy with supraomohyoid neck dissection. Histopathological examination revealed a well differentiated squamous cell carcinoma with squamous lining of pre-existing odontogenic cyst. The criteria for PIOC were fulfilled in our case as initially there was only external swelling of the mandible with intact oral mucosa. The case is rare for its presentation at a young age and initial resemblance to benign pathology.
|
| [ABSTRACT]??[HTML Full text]??[PDF]??[Mobile Full text]??[EPub]??[Sword Plugin for Repository]Beta
|
|
|
|
|
|
|
| COMMENTARY |
 |
|
|
|
Commentary |
p. 165 |
| Marcelo Coelho Goiato |
| [HTML Full text]??[PDF]??[Mobile Full text]??[EPub]??[Sword Plugin for Repository]Beta
|
|
|
|
|
|
|
| CASE REPORT |
 |
|
|
|
Excision of large soft tissue lipoma of cheek through intra-oral approach |
p. 167 |
Harish Saluja, Uma Mahindra, Vikrant Kasat, Vipin Dehane, Rahul K Chaudhari
DOI:10.4103/2278-9588.121853??
Lipomas are common benign soft tissue neoplasms of mature adipose tissue. Most of the lipomas develop in the subcutaneous tissues but deeper tissues may be involved as well. The oral cavity is not commonly affected as the overall incidence in the oral cavity is thought to be between 1% and 5% of all benign oral lesions. Oral lipomas can occur in various anatomic sites including the major salivary glands, buccal mucosa, lip, tongue, palate, vestibule, and floor of the mouth. Although benign in nature, their progressive growth may cause interference with the speech and mastication due to tumour's dimension. The purpose of this article is to report management of a case of large lipoma of right cheek in a 52-year old male which was causing difficulty in mastication as well as embarrassment to the patient.
|
| [ABSTRACT]??[HTML Full text]??[PDF]??[Mobile Full text]??[EPub]??[Sword Plugin for Repository]Beta
|
|
|
|
|
|
|
| COMMENTARY |
 |
|
|
|
Commentary |
p. 169 |
| Hasan Ayberk Altug, Abdullah Tugrul Coskun |
| [HTML Full text]??[PDF]??[Mobile Full text]??[EPub]??[Sword Plugin for Repository]Beta
|
|
|
|
|
|
|
| CASE REPORTS |
 |
|
|
|
Aggressive fibromyxoma of the maxilla |
p. 170 |
Gotike Siva Prasad Reddy, Raj Kumar Badam, Rahul Marshal Vaddeswarapu, Tenneti Venkata Santoshi Harish Kumar
DOI:10.4103/2278-9588.121855??
A fibromyxoma is a rare locally invasive odontogenic mesenchymal tumor found in both the jaws. It is benign and painless but locally destructive and extends into the surrounding structures. The mandible is more commonly involved than the maxilla. Females are more commonly affected than males. The tumor can cause gradual expansion of the cortical plates and cause loosening and displacement of teeth although root resorption may be rare. The surgical treatment of these tumors consists of complete enucleation or radical excision. The aim of this case report is to present the rarity of a fibromyxoma of the maxilla.
|
| [ABSTRACT]??[HTML Full text]??[PDF]??[Mobile Full text]??[EPub]??[Sword Plugin for Repository]Beta
|
|
|
|
|
|
|
An aesthetic and rapid approach to treat midline diastema?
|
p. 175 |
Santosh Kumar, Damini Gandotra
DOI:10.4103/2278-9588.121856??
Maxillary midline diastema is a common esthetic problem of patients which adversely affects body image and self-esteem, especially in adults. Often, patients are more conscious about the spaces between front teeth and seek treatment for cosmetic reasons. Different treatment modalities include restoration, orthodontics, prosthodontics, surgery, and various combinations of the above. Orthodontic procedures are routinely used to close diastema; however, there may be concerns with the appearance of braces especially in adults limiting its use. Here, we describe a case where a clear thermoplastic retainer was modified to close the midline diastema in relatively shorter time period.
|
| [ABSTRACT]??[HTML Full text]??[PDF]??[Mobile Full text]??[EPub]??[Sword Plugin for Repository]Beta
|
|
|
|
|
|
|
| COMMENTARY |
 |
|
|
|
Commentary |
p. 178 |
| Mayuri Thomas |
| [HTML Full text]??[PDF]??[Mobile Full text]??[EPub]??[Sword Plugin for Repository]Beta
|
|
|
|
|
|
|
Commentary |
p. 180 |
| Santanu Mukhopadhyay |
| [HTML Full text]??[PDF]??[Mobile Full text]??[EPub]??[Sword Plugin for Repository]Beta
|
|
|
|
|
|
|
| CASE REPORT |
 |
|
|
|
Atypical odontoma: Report of two cases |
p. 182 |
Sanjay Byakodi, Raghavendra Byakodi, Aparna Aparadh, Praveen Tamannavvar
DOI:10.4103/2278-9588.121863??
Odontomas are the most common type of odontogenic tumors and they are generally asymptomatic. This paper describes two cases of atypical odontomas diagnosed in female patients with unerupted maxillary left central incisor. In both cases, the surgical excision of the lesions was performed. In one case, extraction of the unerupted central incisor was carried out because of its unfavorable orientation, while, in other orthodontic treatment, it was adopted to move the impacted central incisor to its normal position. Treatment and possible mechanisms for development of the condition are discussed. The results achieved indicate that the early diagnosis of odontomas allows the adoption of a less complex and expensive treatment and ensures better prognosis.
|
| [ABSTRACT]??[HTML Full text]??[PDF]??[Mobile Full text]??[EPub]??[Sword Plugin for Repository]Beta
|
|
|
|
|
|
|
| COMMENTARY |
 |
|
|
|
Commentary |
p. 186 |
| Matthias Troeltzsch, Christoph Pache |
| [HTML Full text]??[PDF]??[Mobile Full text]??[EPub]??[Sword Plugin for Repository]Beta
|
|
|
|
|
|
|
Commentary |
p. 188 |
| Mahtab Memarpour |
| [HTML Full text]??[PDF]??[Mobile Full text]??[EPub]??[Sword Plugin for Repository]Beta
|
|
|
|
|
|
|
| CASE REPORTS |
 |
|
|
|
Frontal sinus mucocele causing proptosis |
p. 189 |
Shaila Bangad, Surabhi Chopra, YU Kelgaonkar, Sham S Somani, Sachin B Ingle
DOI:10.4103/2278-9588.121869??
Paranasal sinus mucoceles can present with a multitude of different symptoms including ophthalmic disturbances. We describe a patient with frontal sinus mucoceles presenting with non-axial proptosis and give details of their presentation, investigations and treatment. Possible ocular manifestations of mucoceles and the diagnostic imaging techniques used are discussed. The treatment of mucoceles is reviewed. It is stressed that a team approach involving the Ophthalmologist, Otolaryngologist and Radiologist is essential for accurate diagnosis and management.
|
| [ABSTRACT]??[HTML Full text]??[PDF]??[Mobile Full text]??[EPub]??[Sword Plugin for Repository]Beta
|
|
|
|
|
|
|
Temporalis muscle flap in the management of tubercular osteomyelitis of zygomatic bone |
p. 192 |
Vijay Y Bhatia, Pramod A Menon, Madhavi S Raibagkar
DOI:10.4103/2278-9588.121872??
The tuberculosis (TB) affecting the zygomatic bone is rare and there are only few reported cases in literature. TB of the zygomatic bone has been conventionally treated by anti-tubercular therapy and surgical intervention is rarely required. We report a case of TB of zygomatic bone in a 16-year-old boy on anti-tubercular therapy for pulmonary TB, who presented with swelling of right cheek with a discharging sinus. The patient was managed successfully using a temporalis muscle flap after the removal of the diseased tissue and bone and initiation of category II anti-tubercular therapy. The wound was protected by temporalis muscle flap, to provide vascularized cover and increase local vascularity so that the anti-tubercular therapy can reach the diseased region and also to prevent exposure of the zygomatic bone in case of a wound break down.
|
| [ABSTRACT]??[HTML Full text]??[PDF]??[Mobile Full text]??[EPub]??[Sword Plugin for Repository]Beta
|
|
|
|
|
|
|
| LETTER TO EDITOR |
 |
|
|
|
This harmful practice is still with us: Avulsion of the lower incisors an illustrative case |
p. 197 |
Ibrahim Aliyu
DOI:10.4103/2278-9588.121874?? |
| [HTML Full text]??[PDF]??[Mobile Full text]??[EPub]??[Sword Plugin for Repository]Beta
|
|
|
|
|
|